TCT 2021: Late-breaking Science Video Collection
Published: 09 November 2021
-
Views:
 2269
2269
-
Likes:
 7
7
-
Views:
 2269
2269
-
Likes:
 7
7
-
 Up Next
Up Next -
 4m 40sPart 2 | Session 2 iFR-SWEDEHEART: No Difference in Outcome at 5-yrs of iFR vs FFR
4m 40sPart 2 | Session 2 iFR-SWEDEHEART: No Difference in Outcome at 5-yrs of iFR vs FFR -
 8m 19s
8m 19s -
 7m 32sPart 2 | Session 4 CHOICE-CLOSURE: Plug-based Vs Suture-based Large-bore Vascular Closure
7m 32sPart 2 | Session 4 CHOICE-CLOSURE: Plug-based Vs Suture-based Large-bore Vascular Closure -
 7m 27sPart 2 | Session 5 TRISCEND II: 6Mo Outcomes Show TR Reduction in Majority of Patients
7m 27sPart 2 | Session 5 TRISCEND II: 6Mo Outcomes Show TR Reduction in Majority of Patients -
 8m 8sPart 2 | Session 6 SCB Shows Similar Angiographic Outcomes to Paclitaxel DCB
8m 8sPart 2 | Session 6 SCB Shows Similar Angiographic Outcomes to Paclitaxel DCB -
 3m 37sPart 2 | Session 7 Intrepid TMVR: Results Show Improved NYHA Class at 30 Days
3m 37sPart 2 | Session 7 Intrepid TMVR: Results Show Improved NYHA Class at 30 Days -
 6m 43s
6m 43s -
 4m 44s
4m 44s -
 4m 28sPart 2 | Session 10 BIO-RESORT: 5Y Outcomes
4m 28sPart 2 | Session 10 BIO-RESORT: 5Y Outcomes -
 10m 19sPart 2 | Session 11 OPTIMUM Registry: PCI in Patients at Prohibitive Risk for CABG
10m 19sPart 2 | Session 11 OPTIMUM Registry: PCI in Patients at Prohibitive Risk for CABG
-
 22m 43sPart 1 | Session 1 What's Hot at TCT 2021: View from the Thoraxcenter Nicolas M Van Mieghem, Joost Daemen
22m 43sPart 1 | Session 1 What's Hot at TCT 2021: View from the Thoraxcenter Nicolas M Van Mieghem, Joost Daemen
-
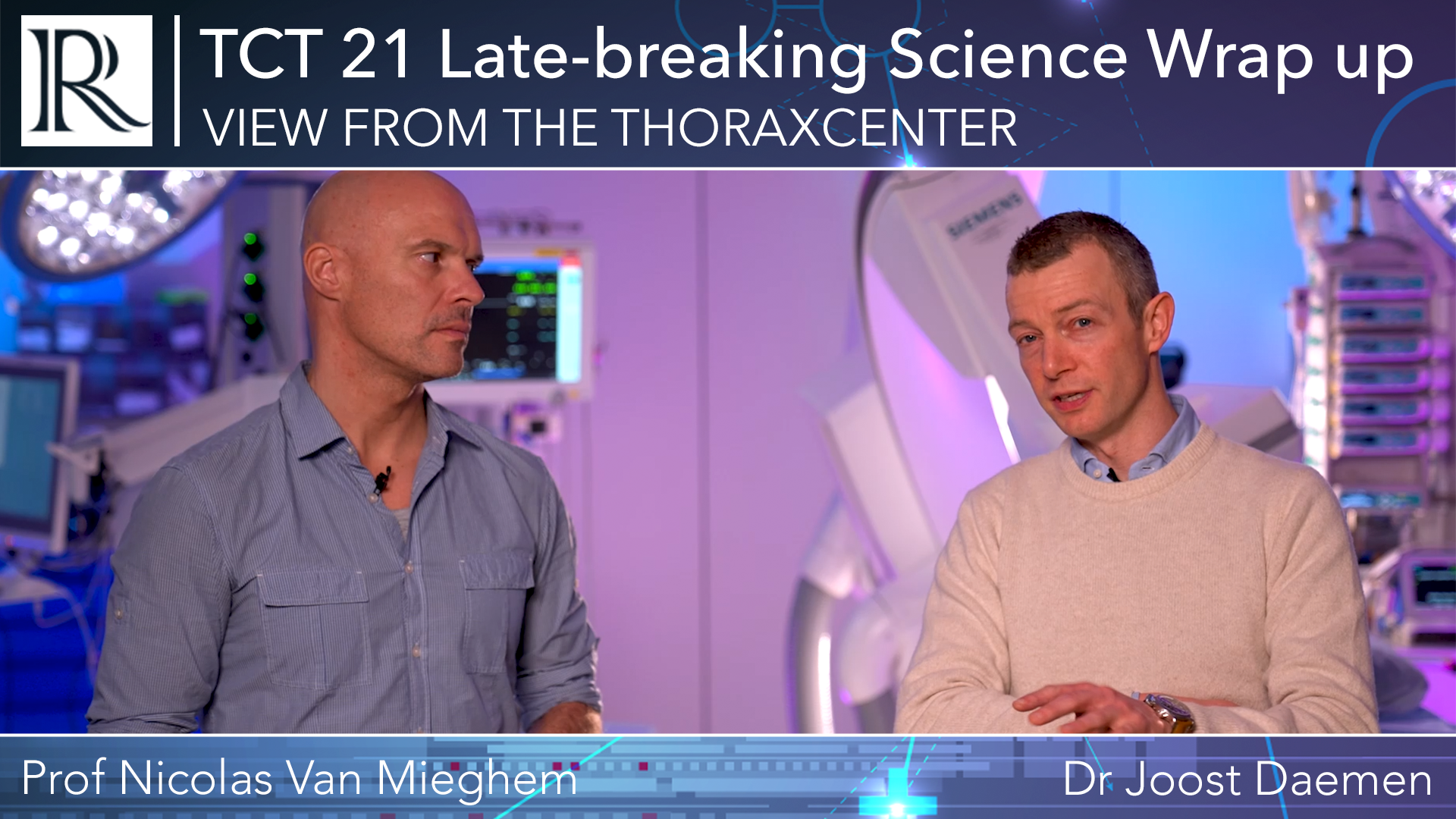 22m 33sPart 1 | Session 2 View from the Thoraxcenter: TCT 21 Late-breaking Science Wrap Up Nicolas M Van Mieghem, Joost Daemen
22m 33sPart 1 | Session 2 View from the Thoraxcenter: TCT 21 Late-breaking Science Wrap Up Nicolas M Van Mieghem, Joost Daemen
Overview
Our regular review series View from the Thoraxcenter hosted by Prof Nicolas Van Mieghem and Dr Joost Daemen (Thoraxcentre, Erasmus MC, Rotterdam, NL) provide a concise and insightful preview of the late-breaking science presented at TCT 2021.
Short, accessible Expert Interviews will be available conducted with select faculty focusing on the results, applicability, and impact on future research.
More from this programme
Part 1
View from the Thoraxcenter: Preview of the Late-Breaking Trials
Part 2
Expert Interviews
Faculty Biographies
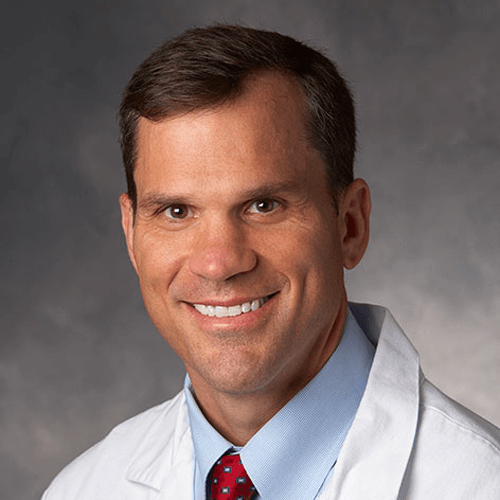
William Fearon
Professor of Medicine, Director of Interventional Cardiology
Dr William Fuller Fearon is a Professor of Medicine and the Director of Interventional Cardiology at Stanford University School of Medicine.
Dr Fearon graduated from Dartmouth College with his Bachelor’s in 1990. In 1994, he received his medical degree from Columbia University College of Physicians and Surgeons, where he was elected into the Alpha Omega Alpha Medical Honor Society.
He completed an Internal Medicine residency at Stanford University Medical Center where he remained for an extra year as a Medical Chief Resident. He completed a General Cardiology and Interventional Cardiology fellowship at Stanford, spending his third year as the Chief Cardiology Fellow.
Dr Fearon’s primary areas of research interest is in coronary physiology and his clinical activities include percutaneous coronary intervention and transcatheter aortic valve replacement.
He was the US principal investigator and senior author of the FAME trial and was a co-principal investigator…
Transcript
Importance of the Trial
FAME 3, the background behind it is that previous studies like FREEDOM or the SYNTAX trial in particular used first-generation drug-eluting stents. And we now have extensive data demonstrating that second-generation or current generation drug-eluting stents lead to lower rates of target lesion and target vessel failure at one year.
So that's one key difference. The other key differences, those previous studies didn't use fractional flow reserve to guide percutaneous coronary intervention or PCI. And we also have a number of studies that have shown the benefit of FFR-guided PCI. For example, the FAME 1 trial, which was a study looking at patients with multi-vessel disease and randomising them between FFR-guided PCI and angiography guided PCI, which was the standard of care at the time, showed significant reduction in major adverse cardiac events using FFR to guide the PCI.
So the key or the hypothesis I should say of FAME 3, was to test whether in patients with three vessel coronary disease, does FFR-guided PCI using current generation drug-eluting stents, is it equivalent or non-inferior to coronary artery bypass graft surgery?
Study Design
So the design of FAME 3 was that it was an investigator initiated trial. Stanford University was the sponsor. It was funded by Medtronic and Abbott through research grants. And it was a multicenter international randomised control study, including 48 sites from North America, Europe, Asia and Australia.
And to be included in FAME 3, a patient had to have a three vessel coronary disease in each of the major epicardial arteries that was at least 50% narrowed based on the angiogram and visual interpretation. And it could not involve the left main coronary and the heart team at each site had to feel that both PCI and cabbage or bypass surgery were reasonable alternatives to revascularize the patient.
There weren't too many exclusion criteria, but some of the major exclusion was a recent STEMI. So within five days an ST Elevation Myocardial Infarction, low ejection fraction, EF, below 30% and cardiogenic shock.
So we enrolled 1500 patients, approximately 750 were randomised to both arms. Some of the key procedural, well, I guess baseline findings were that the average age was around 65. The study included mostly men, about 30% of patients were diabetic and 40% were presenting with an acute coronary syndrome.
The time to procedure in the FFR-guided patients was shorter, shorter than a PCI. The length of the procedure was shorter and the hospital stay was also shorter. As far as other procedural characteristics, FFR was measured in about 82% of patients with about 25% of them having an abnormal FFR. In the bypass surgery group, 97% of patients received an internal, left internal mammary artery graft, and about 25% received multiple arterial graphs, about a quarter underwent off-pump surgery.
And a similar number of lesions were identified in both arms, you know, about three and a half lesions or so, I'm sorry, about four lesions were identified in both groups.
Key Findings
So the major finding, the primary endpoint of the study was a composite of death, myocardial infarction, stroke, or repeat revascularization at one year. And the study was designed as a non-inferiority trial with the hazard ratio of 1.65 being the non-inferiority margin.
And what we found was that the primary endpoint occurred in 10.6% of the patients randomised to FFR-guided PCI and 6.9% randomised to bypass surgery So the hazard ratio was 1.5 with 95% confidence intervals extending from 1.1 to 2.2, meaning that it did not meet the preset criterion for non-inferiority. The p-value was 0.35. That was the major finding.
There were a number of secondary end points that we looked at. For example, we looked at each component of the primary end point like death, myocardial infarction, stroke, and repeat revascularization. And there were no significant differences between the two groups for any of those individual endpoints and the combination of death, stroke and myocardial infarction, was also not significantly different between the two strategies.
Finally, we looked at some safety endpoints and the severe bleeding or acute kidney injury or significant arrhythmia, all occurred more significantly in the bypass group compared to the PCI arm. And the rate of rehospitalization within 30 days was also significantly higher in the bypass arm compared to the PCI arm. Yes.
Implications for Clinical Practice
So there was another important subgroup analysis that we performed that was pre-specified. We looked at the implication of the SYNTAX score, you know, an angiography derived scoring system for determining the complexity of the coronary disease. And prior studies like the syntax trial had shown that low syntax score patients tend to respond better to PCI than high SYNTAX score.
And we found that in FAME 3, we found that patients with a low SYNTAX score, actually the rate of major adverse cardiac and cerebrovascular events in the FFR-guided PCI arm was numerically lower than it was in the bypass surgery arm. Whereas in the intermediate and high risk scores, the reverse was true, bypass outperformed PCI.
So I think that is one important implication of the study. Another important finding was that both groups of patients in FAME 3, both the FFR-guided PCI and the bypass group did markedly better than historic controls. So the SYNTAX trial was set up in a very similar fashion to FAME 3 with the same endpoint one year major adverse cardiac and cerebrovascular events. And what we found was that the patients enrolled in FAME 3 were very similar in characteristics to those in SYNTAX, but interestingly in SYNTAX, in the PCI arm, the MACE rate was almost 18% at one year.
And in the bypass arm, it was just over 12%. And when you compare that to FAME 3, we see that the FFR-guided PCI arm had a rate of 10.6%. So it was well below the PCI arm and SYNTAX, and it was actually numerically lower with a 15% relative risk reduction compared to the bypass arm and syntax.
So the good news is that our treatment of patients with multi-vessel disease has improved dramatically in both patients receiving stenting or bypass surgery.
Who Would Benefit from FFR-guided PCI
So I think this study, FAME 3, provides us with important information that can inform both physicians as well as patients about the pros and cons of FFR-guided PCI versus bypass surgery and allow a shared decision. I think the study showed that in patients with less complex disease, according to the SYNTAX score, FFR-guided PCI is a very reasonable option. In more complex disease, bypass surgery remains the treatment of choice.
Next Steps
Yeah, so I think, you know, one of the limitations of FAME 3 is that we are reporting short term follow up just one year and it will be critical to follow these patients longer. And we will have a report at three years, as well as five years looking at events in the two groups. And I think that'll further inform us about the pros and cons of each approach in these patients.





