It is estimated that 15-20 % of all coronary interventional procedures involve side branches.1 Side branches are frequently related to periprocedural complications. Side branch occlusion or compromise appears to be the underlying cause of approximately 30 % of periprocedural myocardial infarctions.2 Periprocedural infarction in turn is an important predictor of midterm mortality3. Considering any side branches >1 millimetres (mm), clinical studies including complex lesions in the modern drug-eluting stent (DES) era have demonstrated side branch occlusion or reduced flow in approximately 10 % of interventional procedures.2
The above noted does not comprise the left main bifurcation, which can also be regarded as a side branch anatomy. Significant left main disease is observed in 3-5 % of patients undergoing coronary angiography.4 Increasingly, interventional procedures are considered an alternative to surgical revascularisation in unprotected left main disease. As a result of the fast-evolving technical advances, it is impossible to obtain a durable appraisal of the interventional techniques compared with surgery. Yet, recent data suggest interventional left main procedures can markedly improve patient outcome compared with medical treatment.5
The Medina classification is used to describe the distribution of stenoses between main vessel and side branch in the bifurcation lesion.6 In short, a stenosis can affect the proximal portion of the main vessel (proximal to the side branch) or its distal portion, or it can affect the side branch itself. Combinations of either two of these locations are possible as well as stenoses in all three locations. For example, a lesion with stenoses pertaining to the proximal as well as the distal portion of the main vessel, but sparing the side branch, is classified as Medina (1,1,0).
Contemporary Interventional Bifurcation Treatment
Operators contemplating a bifurcation lesion intervention need to determine if the side branch in question is important and needs to be protected. This will in large part depend on its diameter. However, other factors also need to be considered such as the patient's overall condition, whether there is diffuse coronary atherosclerosis or not, and which angulation of the side branch is encountered before and after rewiring. In general, side branches with a diameter ≥2 mm should be protected. Stent implantation in the main vessel may lead to side branch compromise or occlusion due to plaque shift or other mechanisms. Long-term results have been improved with the use of DES compared with bare metal stents (BMS).1 However, even in the DES era it may be very difficult to rewire the side branch once it has been occluded, in particular if the DES in the main branch has a diameter <3 mm and is not well-suited for a wire to re-cross the stent struts. Open-cell or helical stent design will generally allow for a better re-crossing profile compared with a closed-cell design.7
The predominant technique used for bifurcation interventions employs provisional side branch stenting.8,9 The main branch is treated by implantation of a DES. The side branch is rewired (through the stent struts of the DES) and dilatation with a non-compliant balloon is performed. Side branch stent implantation only follows if deemed necessary due to dissection, plaque shift or other forms of severe side branch compromise. The geometry of the main vessel stent is protected either by a kissing balloon approach or by balloon inflation in the main branch after completion of side branch treatment. If a second stent needs to be implanted in the side branch, final kissing balloon inflation is usually performed.9 These basic principles are generally also adopted if dedicated bifurcation devices are employed. Such devices offer the promise of better side branch protection, as they usually allow for facilitated side branch access.
Kissing balloon inflation frequently poses the question of which balloon diameter to choose in order to allow for adequate stent expansion in the main branch without damaging the stent or even the main vessel itself. Morino et al. have proposed a formula to calculate the in vivo diameter of two balloons inflated in parallel in the main vessel:
R2 = D12 + D22
where R is the mean diameter of the two balloons in the main vessel and D1 and D2 are the diameters of the balloons in the main vessel and side branch, respectively.10 For example, using a 3.5 mm balloon in the main vessel and a 2.5 mm balloon in the side branch will result in a theoretical overall balloon diameter in the main vessel of 4.3 mm.
Role of Bioresorbable Vascular Scaffolds
The increased adverse event rate generally observed in bifurcation lesion treatment relates to diverse mechanisms such as incomplete stent coverage of parts of the lesion, several layers of stent struts at other parts, flow-limiting struts across the side branch ostium, or incomplete stent apposition. The Absorb™ Bioresorbable Vascular Scaffold (BVS) is made of poly-L-lactide acid (PLLA), with a strut thickness of 157 micrometres (μm) constructed as in-phase hoops with straight links, eluting everolimus.11 With regard to bifurcation lesions, it may offer several advantages. In particular, there is no long-term risk of stent thrombosis related to uncovered struts. Also, it is more flexible compared with a DES. It will not straighten the vessel and thus is not expected to change the native shear stress distribution. Over the course of 12-24 months, endothelial-dependent vasomotion appears to be restored,12 potentially further reducing the risk of late adverse events. Bioresorbable struts covering the ostium of the side branch have been observed to develop into a neointimal bridge, leaving a smooth ostial contour of the side branch.13,14
First Data on Bioresorbable Vascular Scaffolds Used for Treating Bifurcation Lesions
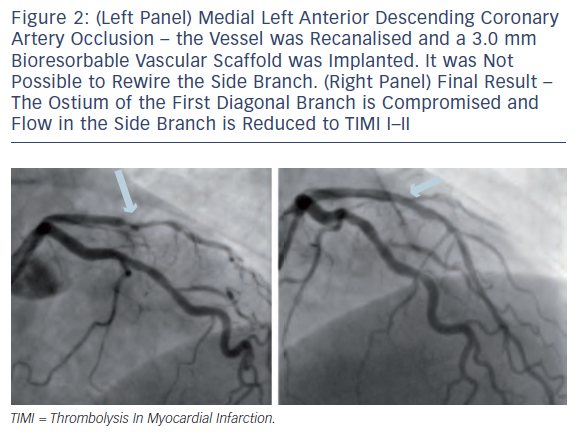
BVS implantation was initially only recommended for simple lesions, avoiding side branch anatomy. There was the concern that after rewiring the side branch, ostial side branch dilatation might damage the BVS. Indeed, in the instructions for use, the manufacturer, Abbott Vascular, warns that lesions with 2 mm side branches should be avoided. At the same time, preliminary data indicate that 1.5 mm and 2.0 mm balloons taken to nominal pressure will not cause mechanical disruption of the BVS. However, a 2.5 mm balloon might cause disruption of the longitudinal crosslinks, but without impacting radial strength.15 Others have suggested that the cells of a 2.5 mm BVS can be crossed with a second wire and be dilated with a non-compliant balloon up to a diameter of 3.0 mm without strut fracture.16 A clinical case report implies it may indeed be possible to carefully dilate side branches without severe structural damage to the BVS in the main vessel.17 Gogas et al. performed a bailout procedure after implantation of a 3.0 mm BVS in the left anterior descending coronary artery (LAD). While the result in the LAD itself was entirely satisfactory, the second diagonal branch, covered by the BVS, showed subtotal occlusion and Thrombolysis In Myocardial Infarction (TIMI) flow grade 1.17 Although the side branch diameter was only 1.7 mm, the patient experienced chest pain, and the operators decided to re-cross the BVS cells. The ostium of the side branch was dilated with a 1.5 mm compliant balloon, restoring normal flow. The immediate angiography result was very good, and an additional analysis by using optical coherence tomography (OCT) confirmed adequate strut apposition and lack of fractures.17
A complex bifurcation lesion was treated by Naganuma et al.18 They recanalised a chronic total occlusion of the left circumflex coronary artery (LCx), placing a wire in the LCx itself and another one in the first obtuse marginal branch (OM1). First, a BVS was implanted in the OM1-ostium. Subsequently, two BVS were implanted in the LCx, covering the ostium of the OM1. Given a very convincing angiographic appearance, the OM1 was not rewired. Post-procedural intravascular ultrasound analysis demonstrated well-apposed BVS struts in the LCx. The OM1 was not separately interrogated.18
What to Expect
It is to be expected that many reports, including series of patients, will follow these preliminary case reports. At the annual European and American interventional meetings, several case reports have been presented, reaffirming the feasibility of treating bifurcation lesions by using BVS. Compared with modern DES, rewiring the side branch is more difficult mainly because of the greater BVS strut thickness. Indeed, it can be even tricky to advance a second guidewire through the BVS within the main vessel, all the more a second BVS. This may indicate that the success rate regarding side branch interventions might be inferior using BVS compared with modern DES. However, once the side branch has been rewired, crossing the BVS cells with a balloon appears to be rather simple. However, it is currently unclear up to what size balloons can be inflated without disrupting the cells of the BVS or impacting its radial strength. Certainly, there is a risk that kissing balloon inflation will damage the main vessel BVS, and it should probably be avoided. If deemed absolutely necessary, moderate balloon sizing and inflation pressures should be chosen. Preferentially, if yearning to protect the BVS from malapposition, sequential balloon inflation should be performed first in the side branch and then in the main vessel (see Figures 1-3).
An important question relates to the necessity of performing side branch dilatation. Will this be needed in a sizeable number of BVS interventions? A recent analysis from the ABSORB-EXTEND (A Continuation in the Clinical Evaluation of the ABSORB Bioresorbable Vascular Scaffold [BVS] System in the Treatment of Subjects With de Novo Native Coronary Artery Lesions) single-arm trial compared the rate of side branch occlusion in 435 patients treated by using BVS implantation to a historic control group of 237 patients with DES (Abbott XIENCE® V) implantation in the SPIRIT first and SPIRIT II (A Clinical Evaluation of the XIENCE® V Everolimus Eluting Coronary Stent System in the Treatment of Patients With de Novo Native Coronary Artery Lesions) trials.19 The angiographic analysis documented a mean of 2.8 side branches in the BVS group and 2.9 in the DES group. Side branch occlusion occurred in 6.0 % in the BVS group and in 4.1 % in the DES group (p=0.09). The incidence of side branch occlusion appeared to depend on side branch vessel diameter. Whereas occlusion was clearly more frequent in small side branches with an angiographic diameter ≤0.5 mm, no statistic difference was observed in larger side branches (see Figure 4).19 These data suggest that with regard to important side branches, the occlusion rates are similar between BVS and modern DES, and the necessity to perform a bifurcation procedure should be comparable.
Conclusion
In summary, first data indicate that BVS behave similar compared with modern DES with regard to compromising or occluding side branches >0.5 mm. Smaller side branches might be compromised more often by BVS implantation compared with DES. It appears to be feasible to dilate side branches after crossing BVS cells, even though it may be technically more demanding compared with bifurcation procedures using solely DES. The safety of side branch dilatations remains open, but preliminary data suggest at least balloon diameters up to 2.5 mm can be used. Instead of kissing balloon dilatation, rather sequential balloon dilatation should be employed. It remains to be seen if BVS will also allow for treatment of rather complex bifurcation lesions. To our knowledge, no reports have so far been published related to BVS left main interventions. Certainly, more data are needed. As of today, BVS offer promise not only for the treatment of simple coronary lesions but also bifurcations. Given successful side branch protection, they might allow for restoring the native coronary anatomy in the sense of restitutio ad integrum.