In the infancy of the hospice and palliative care movements, Dame Cicely Saunders noted that terminally ill patients and their families were often told “there is nothing more to do.” Her unwavering belief was that those words betrayed the patient, and that “there is so much more to do.”1
Stage D heart failure (HF) is defined as HF in which refractory symptoms persist despite guideline-directed therapies.2 This stage of HF is highly morbid and is associated with a high burden of both physiologic and psychological suffering.3 Advances in care of cardiovascular diseases and an aging population have contributed to a burgeoning number of patients with Stage D HF. Current estimates of the number of patients who die from HF is approximately 60,000 per year versus approximately 300,000 per year who die with HF in the US (with a similar number in Europe).4 The fields of cardiology and palliative care have begun to recognize and address the complex needs of these patients. Their collaborative efforts have resulted in a growing body of literature aimed at providing guidance for practitioners caring for this population.5 This review will provide practitioners with focused recommendations for the care of individuals with HF who are nearing the end of life.
Decision-making
Providers have varying degrees of comfort with the provision of end-of-life care in HF.6 At or near the end of life, 52 % of providers hesitated to discuss end-of-life care, due to provider discomfort (11 %), perceived unreadiness on behalf of the patient or family (33 %), fear of destroying hope (9 %), or lack of time (8 %). Furthermore, 30 % of these providers reported low or very low confidence in initiation of the discussions, enrolling in hospice, or providing end-of-life care. Opinions differ among providers about whose responsibility it is to address end-of-life care in patients with HF, with 66 % of cardiology providers citing that the responsibility is that of the primary care physician (PCP), while 57 % of PCPs believe the converse. We suggest that all providers should review preferences and planning for the end of life with HF patients and that any invested provider may initiate end-of-life care. Decision-making for end-of-life matters should be patient-centered and should be a collaborative effort between providers, patients, and involved family and friends of the patient. The decisions needing to be made at the end of life generally fall under the umbrella of an advance care plan (ACP).
Realistically, a large number of patients will die without either a well-thought-out ACP and signed advance directive (AD), however, the exercise of going through these questions with patients may help them to formulate opinions regarding their end-of-life care. Having an ACP and AD can help to alleviate anxiety, increase hospice utilization, and decrease the use of life-prolonging and invasive therapies at the end of life.7 The first step in helping a patient to create an ACP is to understand the patient’s goals and values. The next step is to inform the patient that they are nearing the end stage of the disease process and review reasonable treatment options in the context of their stated values and goals. Specific topics that should be addressed in a complete ACP, as well as useful language, are found in Table 1. Importantly, the ACP should be an iterative process, and should be readdressed throughout the course of illness, as patient preferences can change as their illness worsens.8
The use of device-based therapies, such as implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy, for HF is becoming integrated into the care of a greater percentage of patients, with over 50 % of patients with HF qualifying for device-based therapy.9 Challenges encountered by providers initiating
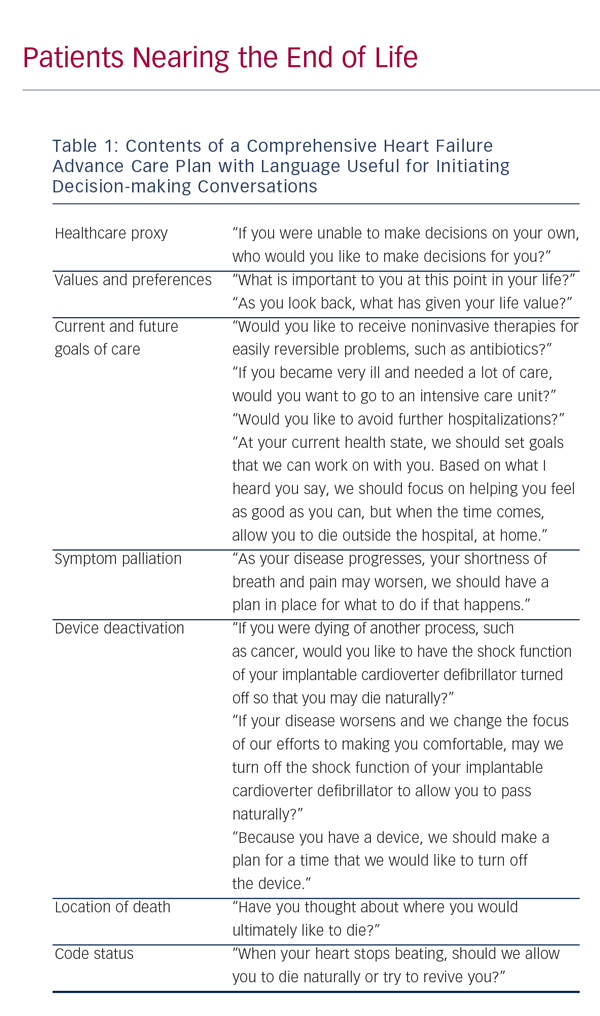
conversations regarding device deactivation can be due to provider discomfort, lack of counseling prior to implantation, and patient misconceptions.10–12 However, ICD discharges at the end of life are associated with pain and anxiety at the end of life and should be averted. To that end, a plan should be in place for device deactivation for every patient. Planning for device deactivation should start before implantation, but findings from the Multicenter Automatic Defibrillator Implantation Trial II (MADITII) cohort suggest that using clinical status changes (such as hospitalization or changes in functional status) to prompt discussion regarding deactivation may not expose the patient to additional risk for shocks at the end of life.13 Deactivation of mechanical circulatory support is equally important to plan for, but will not be discussed in this review.
Symptom Management
Patients with HF nearing end of life are likely to encounter worsening of symptoms or development of new symptoms. The goal of palliative care is to lessen suffering in all forms: physical, psychological, social, or existential; recognition of each of these forms of suffering as a contributor to suffering is called the theory of “total pain.”1 A comprehensive approach to care addresses each of these forms of suffering in the dying patient. Whereas the transition to palliative care in other disease processes is marked by the removal of potentially curative or otherwise aggressive therapies, the transition to palliative care in those with HF should be additive.14 The key is to medically optimize to the fullest extent achievable with guideline-based medical therapy and then to add therapies directed at the underlying root cause of symptoms that are still present after traditional medical therapy has been exhausted.15
As patients with end-stage HF experience a high burden of symptoms, a multidisciplinary care team may be beneficial.16 This team usually involves both a PCP and a cardiologist, social work, nursing staff, and also, perhaps, a palliative care specialist. A randomized study of 232 patients admitted with HF at a tertiary referral center found that inpatient palliative care consultation improved symptoms burden (p<0.001) and quality of life (p<0.001) at serial follow-up.17
Dyspnea
Dyspnea is a defining feature of functional class for HF patients and is a hallmark of worsening functional status. The pathogenesis of dyspnea in HF is defined by overactivation of ergoreceptors, which are afferent nerves sensitive to the metabolic effects of muscular work.18 Exercise, particularly thigh muscle strengthening, improves dyspnea, presumably by altering the myopathy and ergoreflex abnormalities in persons with HF.19 In a recent study of 100 consecutive patients with New York Heart Association (NYHA) functional class II–IV HF exercise was shown to improve dyspnea, peak VO2 (28 %; p=0.001) and quality of life (p=0.003).20 For these reasons, exercise should be the initial prescription for dyspnea. Maintenance of euvolemia improves, but does not eliminate, dyspnea. It is also important to continue (when able) guideline-directed medical therapies including angiotensin converting enzyme (ACE) inhibitors, beta-blockers, and mineralocorticoid antagonists. Once traditional medical therapies and nonpharmacologic therapies have been exhausted, low-dose opioids are generally felt to be first-line adjuvant therapy to treat dyspnea. Opioids decrease chemosensitivity-related dyspnea and improve exercise tolerance and peak VO2.21 Sedation may be an untoward effect, and thus the dose should be titrated to symptom relief while attempting to avoid narcosis.
Physical Pain
Up to 75 % of patients with advanced HF will experience pain.22 Nonpharmacologic therapies for pain, such as physical therapy, massage, and ice should be attempted first.23 Of the non-opioid pain medications, acetaminophen has the most favorable safety profile for patients with HF with mild to moderate somatic pain.24 Nonsteroidal anti-inflammatory drug (NSAIDs) are contraindicated in patients with HF due to propensity for causing fluid retention and exasperating renal dysfunction. Many NSAIDs, such as cyclooxygenase (COX) inhibitors, also carry black box warnings for patients with cardiovascular disease. Oral opiates may be used for management of moderate to severe pain in patients with HF. Attention should be paid to active metabolites that may accumulate in renal dysfunction, leading to delirium, or neuroexcitation. Fentanyl and methadone have no renally excreted active metabolites likely to accumulate in HF. If providers are uncomfortable with utilization of more potent opiates, consultation with a pain or palliative care specialist may be useful. Unrecognized psychological, social, and spiritual needs will often explain a nonresponding physical pain.25
Depression and Anxiety
Depression is common in those with HF.26 As functional status worsens, the incidence of depression increases: up to 42 % of patients with NYHA class IV disease experience this symptom.27 Comorbid depression is also associated with worsening of HF symptoms.28 Depression can contribute to poor adherence that can increase symptomatology,
hospitalizations, and, ultimately, mortality.29–31 Selective serotonin re-uptake inhibitors (SSRIs), such as sertraline and paroxetine, have been found to be safe and effective as first-line therapy for depression in patients with HF.32,33 These medications should be started at a low dose and increased until depression improves or until recommended dose is achieved. Because both of these drugs are metabolized in the liver and excreted by the kidneys, dose reduction may be required for both renal and hepatic dysfunction.34 SSRIs can cause hyponatremia or fluid retention, particularly in patients with renal dysfunction. In addition to medical therapies for depression, exercise can result in modest improvements in depressive symptoms.35 Collaborative care is an important component of the care patients with HF who develop symptoms of depression.36 Some data suggest that cognitive behavioral therapy can decrease depressive symptoms, as well as anxiety, and that relaxation exercises with elements of CBT may decrease symptom burden.37
Existential Pain
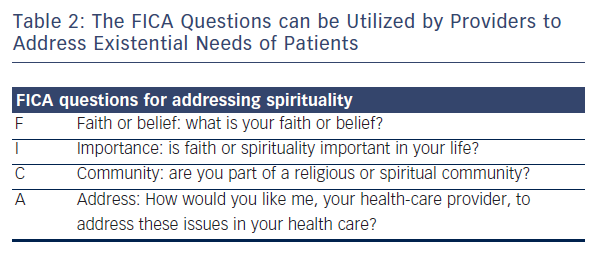
Spiritual well-being is an important component of holistic care. Though often equated to faith, spirituality is a broader term that refers to the way that a person views the meaning of their life in terms of their own values.38 Objective spirituality scoresinclude meaning of life, peace, purpose, and faith.39 Higher spirituality scores appear to confer some degree of protection against the development of depression.40 Clinicians can identify spiritual beliefs and sources of support by simply asking “What gives you hope and where, or how, do you find support in your life?” The FICA questions (see Table 2) can also help guide discussions about spirituality.41
Cognitive Impairments with Heart Failure
Cognitive impairment at the end of life is extremely prevalent in patients with HF and can impair a patient’s ability to interact with family and friends as well as impair independence.42 Patients with decompensated HF can experience difficulty with short-term memory, working memory, executive control and processing speed. Executive dysfunction and
memory problems interfere with self-care and problem-solving, though many patients seemingly converse normally despite moderate-to-severe impairment. Cognitive function can improve with improved volume status, but is unlikely to resolve. Exercise has been shown to improve vascular dementia.43 While many patients retain the ability
to discuss options and may express their preferences, it is important to
include their designated surrogate decision-makers in planning care.
Functional Management
The functional decline towards death is often slow and lasts many years. Patients and families need additional support such as assistance with medication management, self-care, home care, and activities of daily living (ADLs) as they approach the end of life. Attention to functional needs of the patient is important for both patients and care-providers who may experience significant care-giver fatigue and burnout.44 Knowledgeable home health providers can help patients to avoid hospitalizations. Physicians caring for HF patients should develop a network of skilled community partners with whom to work. It can be difficult to estimate when HF patients have a 6-month life-expectancy, but the combination of HF with several other significant medical problems, or recurrent volume overload and a decision to not be hospitalized again are some indicators of hospice appropriateness. Because HF care differs significantly from cancer care, which is what hospice care is modeled on, it is important to build HF care with one or more hospice companies.
Summary
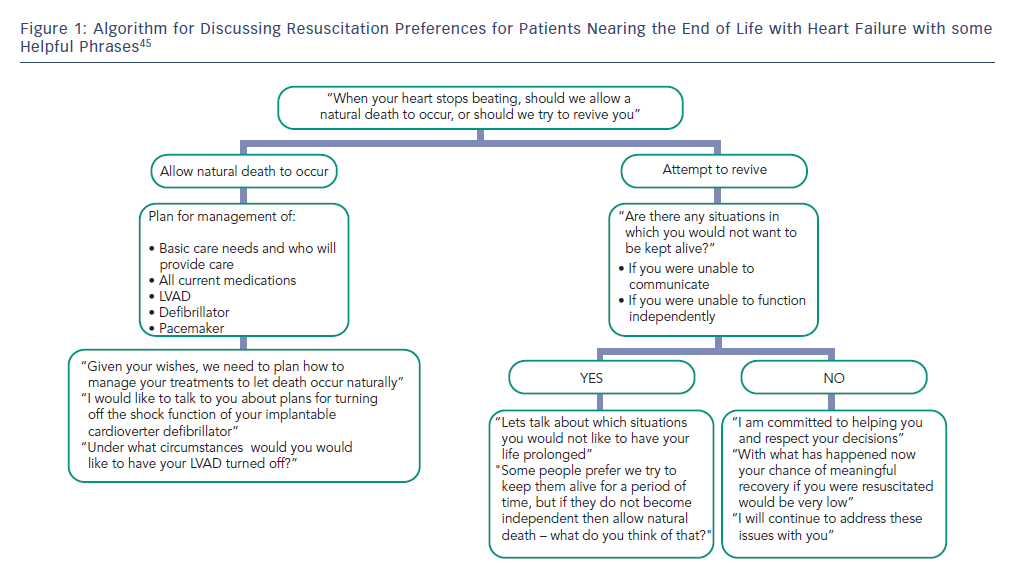
As a patient transitions to the end of life with HF, there is “so
much more to do.” A provider can best address the complex needs of these patients by having a thoughtful ACP in place and by adhering to the theory of total pain (see Figure 1). Though this document is by no means a comprehensive guide to the end-of-life care of these patients, the above should serve as a starting point to inform providers caring for this special population of patients.






