Introduction
The Brugada syndrome (BrS) is a hereditary arrhythmia syndrome manifesting as recurrent syncope or sudden cardiac death (SCD) due to polymorphic ventricular (VT) or fibrillation (VF) in the absence of overt structural heart disease or myocardial ischaemia.1,2 The prevalence of the syndrome is estimated at around 15 per 10,000 in South East Asia including Japan and around 2 per 10,000 in the Western countries.3,4 The BrS may be responsible for up to 4 % of all sudden cardiac deaths (SCD) and at least 20 % of SCDs in patients with structurally normal hearts.5 It is 8–10 times more prevalent in males than in females6 and males are at considerably higher risk of dying suddenly.7 In South-East Asia, the BrS is the leading cause of non-traumatic death in men younger than 40 years.8 This review will briefly summarise current knowledge about the BrS with emphasis on the methods for diagnosis and risk assessment.
Cellular Mechanisms of the BrS
BrS is considered a heritable autosomal dominant disease9 and more than 390 mutations have been identified in the SCN5A gene encoding the α-subunit of the cardiac INa-channel.10 However, presently SCN5A mutations are found only in 11–37 % of the genotyped patients.7,11 Recent data has suggested that heritability may be related to common genetic variation instead of being strictly monogenic.12 Many patients with the BrS have no family history presumably due to under-diagnosis in the other family members, low penetrance or sporadic disease.13
The cellular basis of the BrS is still not fully understood.14 According to the “repolarisation theory”, reduction of the inward Na+ current leads to unopposed transient outward (Ito) current in some epicardial regions of the right ventricular outflow tract (RVOT), which causes either delayed expression of the action potential (AP) dome and epicardial AP prolongation or loss of the dome and AP shortening. The net effect is a potentially arrhythmogenic magnification of repolarisation dispersion between the RVOT endo- and epicardium, and between different RVOT epicardial regions. The repolarisation theory was initially promoted on the basis of experimental studies15,16,17 and was later supported by clinical data such as “spike and dome” configuration with deep notching of monophasic action potentials (MAP) from the RVOT epicardium but not endocardium,18 paradoxical shortening of the RVOT epicardial activation-recovery intervals (ARI) during augmentation of Brugada-type ST segment elevation,19 steep AP duration restitution (slope >1) in the RVOT20,21,22 (both clinically and experimentally), longer ARI in the RVOT epicardium recorded from the conus branch of the right coronary artery than in the endocardium of patients with BrS and type 1 ECG pattern but not in controls23 and others.
There is also mounting evidence from experimental,22 histopathological,24 computational,25 clinical electrophysiological23,25 and imaging26 studies for the presence of conduction abnormalities in the RVOT and their importance for the genesis of ventricular arrhythmias in BrS22,23 (“depolarisation theory”). Delay of the RVOT activation relative to the rest of the RV has also been proposed as a mechanism of the Brugada type ECG changes on the surface ECG.27 The presence of late potentials and prolonged filtered QRS duration on signal-averaged ECG (SAECG) as well as increased notching and fragmentation of the QRS on the standard ECG are linked to increased arrhythmic risk in BrS.28,29,30,31 The reported cases of patients presenting with both arrhythmogenic right ventricular cardiomyopathy (ARVC) and BrS with SCN5A mutations,32 further attest to the likely role of conduction abnormalities in the BrS. A third hypothesis unifying the above two explains the BrS with abnormal expression of the neural crest cells during the embryological development of the RVOT. This defect in the embryogenesis of the RVOT leads to both abnormally augmented electrical gradients during repolarisation as well as to delayed activation of the RVOT.33
From electrocardiographic point of view, the characteristic elevation of the J point and ST segment of the type 1 Brugada ECG pattern (see below) results from early relative (intracellular) positivity of the unaffected zone (RVOT endocardium according to the “repolarisation theory” or normally activated myocardium outside the RVOT according to the “depolarisation theory”), whereas the negative T wave is an expression of late epicardial relative (intracellular) positivity in the affected RVOT zone due to either prolongation of the epicardial APs or its delayed activation.
Clinical Manifestations of the BrS
The symptoms associated with the BrS are due to re-entry ventricular arrhythmias typically arising in the affected zone of the RV. If they last briefly (seconds) and terminate spontaneously they can be asymptomatic or cause palpitations; longer arrhythmias lead to syncope or nocturnal agonal respiration, or can degenerate into VF and cardiac arrest. The duration of the arrhythmia is unpredictable with currently available methods and every arrhythmic episode can be fatal. Therefore, the assessment of the degree of arrhythmic risk and the need for prophylactic treatment is by far the most important aspect of the management of these patients.
The Electrocardiogram – a Key to the Diagnosis of the Brugada Syndrome
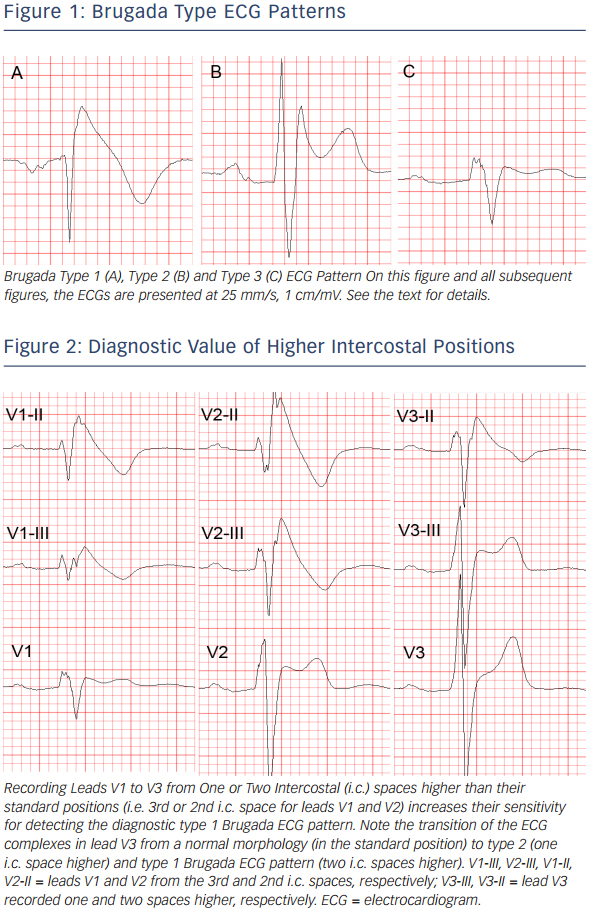
The standard 12-lead ECG (with some additional modifications, as explained below) is crucial for the diagnosis and likely also for determining the prognosis (i.e. the level of arrhythmic risk) in the BrS. The diagnostic hallmark of syndrome is the so-called “coved” or “type 1 Brugada ECG pattern” characterised by J-point elevation with slowly descending or concave ST segment elevation merging into a negative or reaching the isoelectric line symmetric T wave7,34 (see Figure 1A). The type 1 Brugada ECG pattern is observed most frequently in leads V1 and V2, much less frequently in lead V3.35 When type 1 Brugada ECG pattern is observed in lead V3 it is always accompanied by the same ECG pattern in at least one more right precordial lead (unpublished observations).
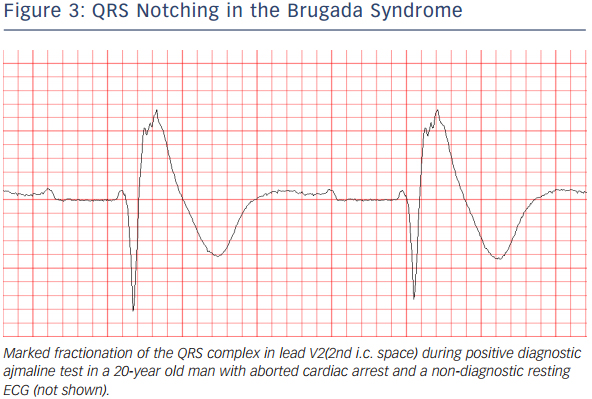
In patients investigated for the BrS, leads V1 and V2 should always be recorded both from the 4th intercostal (i.c.) space as well as from the 3rd and 2nd i.c. space, because the “high” positions increase the sensitivity of leads V1 and V2 for detecting type 1 pattern without loss of specificity36 (see Figure 2). This has been noted already in 1960,37 long before the discovery of the Brugada syndrome. Since the exact anatomic relation between RV and the thoracic cage is individually specific and any of the three i.c. spaces could be closest to the RVOT, it is best to record simultaneously leads V1 and V2 in the 4th, 3rd and 2nd i.c. space. One small study with cardiovascular magnetic resonance imaging found that the maximum RVOT area was most frequently in the 3rd followed by the 4th and 2nd i.c. space.38 In our experience, when type 1 Brugada pattern is observed in the 4th i.c. space it is always also observed in the 3rd or 2nd i.c. space whereas the converse is not the case (unpublished observations). Positioning lead V3 one or two i.c. spaces higher also increases its sensitivity to detect type 1 pattern (unpublished data) (see Figure 2). Bipolar precordial leads between the V2 electrode (positive pole) and V4 or V5 electrodes (negative pole) which can be computed from the standard unipolar leads V2, V4 and V5 seem to be more sensitive and equally specific compared to the unipolar lead V2 for detecting the diagnostic type 1 Brugada ECG pattern.39 Type 1 Brugada ECG pattern sometimes also can be observed in the inferior40,41,42,43 or lateral44,45 leads (the so-called “atypical” BrS).
Another ECG pattern of J point and ST segment elevation with a positive T wave in the right precordial leads, the so-called “saddleback” pattern, is considered suspicious but not diagnostic of BrS, unless converted into type 1 pattern following administration of Na+ channel blocking agents. Traditionally the “saddle back” patterns are further divided into “type 2” and “type 3” Brugada ECG pattern depending on the level of J point and ST segment elevation2 (see Figure 1B,C). A recently published expert Consensus Report on the ECG characteristics of the BrS proposed “type 2” and “type 3” patterns to be unified into one “saddle-back” Brugada pattern because, according to the authors’ opinion, the small morphological differences between the two patterns had no diagnostic or prognostic significance.34 In the latest HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes published in December 2013,7 however, type 2 and type 3 Brugada ECG patterns are still mentioned separately.
Up to 40 % of patients with the BrS present with normal or nondiagnostic resting ECG.46 In these patients, the diagnostic “coved” ECG pattern can be elicited by i.v. administration of sodium channel blocker (ajmaline, procainamide, flecainide).47,48 Currently the BrS is definitely diagnosed when type 1 pattern is observed in at least one of leads V1 and V2 recorded from the 4th, 3rd or 2nd i.c. space either spontaneously or following administration of Na+channel.7 The presence of gene mutations is not considered essential for the diagnosis.2,7
It is important to distinguish between type 2 Brugada ECG pattern and the r’or R’-pattern (incomplete right bundle branch block (iRBBB) pattern) in leads V1 and V2 (especially when recorded from the 3rd or 2nd i.c. space) which can be observed in healthy subjects (frequently in athletes49). It has been reported that a broader angle between the ascending and descending limb of the r’/R’-wave50 or a broader base of the triangle formed by the two limbs of the r’/R’-wave measured at 5 mm from the highest point51,52 can reliably distinguish type 2 Brugada ECG pattern from IRBBB pattern. The classical diagnostic type 1 Brugada ECG pattern needs to be distinguished from similar “Brugadalike” patterns caused by RBBB, septal hypertrophy, arrhythmogenic right ventricular cardiomyopathy (ARVC), pectus excavatum and other conditions, and also from the transient appearance of typical Brugada pattern in the cause of various acute processes such as acute ischaemia, Prinsmetal angina, pulmonary embolism, pericarditis, metabolic disorders, various medications and others (the so-called “Brugada phenocopies”,53 see www.brugadaphenocopy.com). The ECG characteristics of the BrS and the methods to distinguish them from other conditions presenting with similar ECG changes are reviewed in great detail in the above mentioned ECG Consensus Report.34
ECG acquisition with inappropriate high-pass filtering (e.g. non-linear phase high-pass filter of 0.5 Hz instead of the recommended 0.05 Hz)54 can cause considerable ST segment distortion and even mimic type 1 or 2 Brugada pattern.34,55,56
The ECG in BrS characteristically shows considerable dynamic variability; it can be completely normal at one time and demonstrate diagnostic type 1 pattern at another. Vagal influences (slow heart rate, post-prandial state, nighttime) tend to augment the J point and ST segment elevation and the type 1 pattern,57 whereas exercise and catecholamine infusion tend to have the opposite effect (however, in some BrS patients the ST segment elevation might become more prominent during exercise).58 Autonomic influences play important role also in the genesis of malignant arrhythmias because most of the arrhythmic events in BrS occur at night, two long RR intervals often precede episodes of VT/VF,59 whereas catecholamine infusion is used as a first line treatment of such episodes.60 Patients with BrS have increased incidence (10–53 %) of atrial fibrillation (AF).61,62 Additional ECG findings which support the diagnosis of the BrS in asymptomatic patients with spontaneous or induced by Na-channel blockers type 1 pattern include the presence of atrial fibrillation, atrio-ventricular or intraventricular conduction abnormalities (first degree A-V block, fragmented and/or prolonged QRS, abnormal signal-averaged ECG (SAECG), left axis deviation of the QRS complex, prolonged HV interval), ventricular ectopic beats with left bundle branch block (LBBB) morphology and short (<200 ms) ventricular effective refractory period.7
Assessment of the Arrhythmic Risk – the Most Important Clinical Problem in the Brugada Syndrome
The identification of BrS patients with high arrhythmic risk especially among those without previous history of arrhythmia-related symptoms is currently the most important and yet unresolved clinical problem in the BrS. In some aspects, this problem is similar to one of the main (also still not fully resolved) problems of modern cardiology – the identification of patients with ischaemic heart disease (IHD) at high risk of dying suddenly who need prophylactic implantable cardioverter-defibrillator (ICD).
In BrS patients with a previous history of arrhythmic syncope or aborted cardiac arrest the annual event rate of sustained VT or VF is relatively high – between 1.9 %63 and 8.8 %64 and between 7.7 %62 and 13.8 %63, respectively. It is universally accepted that those with aborted cardiac arrest or documented spontaneous sustained VT (with or without syncope) should receive an ICD which is the single therapy with proven efficacy (Class I indication, “…is recommended”).6 There is also evidence that patients with spontaneous type 1 pattern and syncope judged to be of arrhythmic origin (“intermittent risk” group) also are indicated for ICD implantation (currently class IIa indication, “…can be useful.”), whereas asymptomatic patients with spontaneous type 1 pattern are currently considered to represent a “low risk” group (class IIb indication, “…may be considered” depending on the presence or absence of other, not yet fully established risk factors, see below).6 A very recently published Japanese multicentre study confirmed the difference in the level of risk between the latter two patient groups (2.2 % vs 0.5 % during a mean follow-up of 62 months).65
However, the decision to offer an ICD even to a BrS patient with a syncope of presumably arrhythmic origin often is difficult because unlike IHD patients, most of them are relatively young, apparently healthy and without any previous awareness of cardiac problems. Most importantly, it is often very difficult to exclude non-arrhythmic cause of the syncope. In addition, the rate of ICD-related complications (20–30 % annually including inappropriate shocks) is higher than the rate of appropriate activation of the device (2.6–8 % annually).66,67,68 This suggests that novel, better methods of risk-stratification could benefit even some symptomatic BrS patients (i.e. those with the current class IIa indications).6
The majority of BrS patients (64 % in the largest reported series of 1029 BrS patients, the France, Italy, Netherlands, Germany (FINGER) study62 and 63 % in the report of the Brugada syndrome investigators in Japan69) have no symptoms at the time of establishment of the diagnosis. The annual rate of SCD or sustained VT in these patients is low – between 0 %70,71 and 0.872 (0.5 % in the FINGER study62 and the Japanese multicentre study,66 0.4–1 % in several Japanese studies73,74,75) and cannot justify ICD implantation in all of them. On the other hand, the majority of the patients in this heterogeneous group have generally structurally normal hearts and are young or middle aged when diagnosed (median age 45 years in the FINGER study), and therefore the low annual risk can translate into a considerable cumulative arrhythmic risk for the next several decades of their life expectancy. In fact, the majority of victims of SCD in BrS come from this “low risk” (according to current standards) population. One study showed that among patients with the BrS who have died suddenly 68 % had no previous history of arrhythmia-related symptoms and therefore had not been protected by ICD.13 Currently, there are no firmly established reliable methods for the identification of these patients. Similarly, the largest absolute number of patients with IHD who die suddenly also comes from a large patient population considered to have generally low risk (i.e. post-myocardial infarction patients with relatively preserved left ventricular ejection fraction).76
While some studies77,78,79 reported increased occurrence of arrhythmic events in BrS patients with SCN5A mutations these findings have not been confirmed by other studies.80 The genetic analysis is expensive, time-consuming and available only in specialised centres. The role of programmed ventricular stimulation (PVS) during EPS for induction of VT has been an object of controversy and debate since the 1990s. While some early studies supported its value for risk stratification mainly due to its high negative predictive value,81,82 most recent studies failed to confirm its independent predictive value.66,83,84 In the FINGER study,62 inducibility during EPS also did not predict arrhythmic events in multivariate analysis whereas in the multicentre PRELUDE study which tested uniform protocol of PVS during EPS in all 308 patients, the rate arrhythmic events during an average follow-up of three years was not significantly different between the 126 inducible (3.9 %) and the 182 non-inducible patients (4.9 %).85 Currently its role of EPS for risk stratification is accepted only as a Class IIb (“may be considered”) indication.7,86 The method is inherently limited by its invasive character and probably also by the labile nature of the underlying electrophysiologic substrate.87
ECG-derived Parameters for Risk Assessment
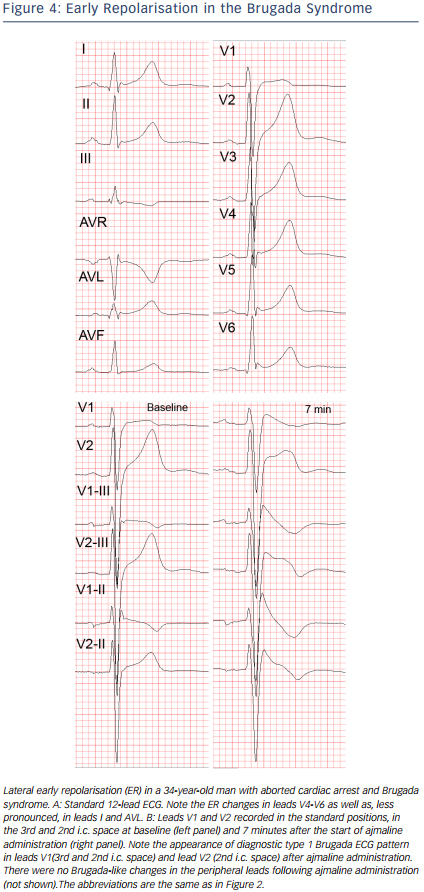
Similarly to other diseases with intraventricular conduction abnormalities such as IHD and cardiomyopathies, the presence of notched or fragmented QRS,31,83 (see Figure 3) has been consistently demonstrated to indicate increased arrhythmic risk independently of other clinical and ECG variables (HR 4.9, 95 % CI 1.6-15.4 in the PRogrammed ELectrical stimUlation preDictive valuE (PERLUDE) study).85 However, currently the presence of notching/fractionation is assessed only visually using arbitrary descriptive criteria (e.g. number of QRS peaks). The presence of late potentials on the signal-averaged ECG (SAECG) is another marker of intraventricular conduction disturbances which also indicates increased arrhythmic risk in BrS30 independently of QRS fractionation. The standard time-domain SAECG, however, cannot detect conduction abnormalities within the QRS complex, has uncertain value in patients with bundle branch block, and uses only a single-lead ECG complex which is derived from the XYZ orthogonal leads and does not contain any regional information.
Among asymptomatic BrS patients, those with Brugada ECG pattern in the infero-lateral leads in addition to the right precordial leads,88 (increased “spatial Brugada burden”) were recently demonstrated to have several times higher risk of VF compared to those with Brugada type 1 changes only in the right precordial leads.89 On the other hand, the number of right precordial leads displaying type 1 pattern and the degree of J-point or ST-segment elevation do not seem to correlate with the arrhythmic risk.35,36 The “high” (3rd or 2nd i.c. space) positions of leads V1 and V2 are diagnostically more sensitive than their standard positions in the 4th i.c. space90,91,92 but prognostically their value is the same.93
Infero-lateral early repolarisation (ER) (see Figure 4) is not only more common (up to 15 %94) in BrS patients,70,94,95 but also carries up to 4-fold increased risk of spontaneous VF67,70 and even higher risk if the ER has “malignant” morphology,96 i.e. is associated with horizontal/descending (as opposed to rapidly ascending) ST segment after the J point.68,75 The combination of infero-lateral ER and fractionated QRS complex seems to indicate indicate a particularly high arrhythmic risk.97
Currently there are only limited data suggesting that other ECG parameters may indicate increased arrhythmic risk. These parameters include changes in repolarisation dynamics (QT/RR and Tpeak-Tend/RR intervals relations),98 deep negative T wave in lead V1,99< QTc interval more than 460 ms in lead V2 and prolonged Tpeak-Tend interval,100 dynamic alterations in the amplitude of the ST elevation,101 prolonged PR-interval,93 presence of atrial arrhythmias,60,61,102 and augmentation of the ST segment elevation during the early recovery phase of exercise test.103
Summary – Risk Stratification in the Brugada Syndrome – Current Status and Future Diretions
Whereas the diagnosis of the BrS is relatively straightforward with currently available ECG-based methods, the identification of high risk patients who need prophylactic ICD implantation is still an unresolved issue. Currently the only class I indications for ICD implantation in patients diagnosed with the BrS endorsed by the 2013 HRS/EHRA/ APHRS Expert Consensus Statement7 is history of aborted cardiac arrest or documented spontaneous sustained VT, whereas syncope judged to be likely of arrhythmic origin is only a Class IIa indication which mainly reflects the difficulty of excluding a non-cardiac origin of syncope. The guidelines of the Japanese Cardiac Society of 2011 accept practically the same Class I indications whereas for Class IIa indication they require the presence of at least two of the following risk factors: history of syncope, family history of sudden cardiac death and inducible VF during EPS.104 Obviously, these guidelines do not offer solution to the problem of identifying the high risk asymptomatic patients with the BrS. Strict adherence to the HRS/EHRA/APHRS guidelines means that each year in the UK alone, approximately 40 asymptomatic BrS patients are likely to experience their first and potentially lethal arrhythmic event without ICD protection (assuming 0.5 % annual rate in asymptomatic patients [approximately 2/3 of all BrS patients] × estimated 12,600 (2 per 10,000) BrS patients in the UK). Clearly, there is a pressing need to develop novel, easily applicable (e.g. ECG based) risk stratifiers (or combinations thereof) and to confirm prospectively the value of the most promising available ones (e.g. QRS fractionation, infero-lateral ER, possibly others).
Obvious obstacles along the path to this goal are the low rate of arrhythmic events (i.e. end-point events in prospective studies), the small number of patients in the individual centres (since the prevalence of the disease outside South-East Asia is generally low), difficult organisation of big multicentre prospective studies and, possibly, inherent differences between various patient populations (e.g. Western vs Japanese).66 Less appreciated obstacle is the fact that currently ECG research studies (as well as everyday clinical practice) still use mainly 12-lead paper ECGs (or digital ECG images) which are amenable only to visual assessment and simple manual measurement. Computerised mathematical methods for quantitative assessment of QRS and ST-T wave abnormalities have been developed and successfully tested in various cardiac diseases105,106 but they require the availability of digital ECGs (digital files containing the raw ECG signal and not just digital image files). Finally, the development of sustained VT/VF in the BrS is likely a complex event resulting from interaction between the arrhythmic substrate (repolarisation and depolarisation abnormalities) and various triggering and modifying factors (e.g. ventricular ectopic beats, atrial arrhythmias, autonomic modulations such as vagal surge, fever, etc.).14,107,108 Therefore a successful ECG-based risk stratification in BrS should likely involve the combined quantitative assessment of several most important elements of arrhythmogenesis.