Proceedings of two satellite symposia held at EuroPCR, Paris in May 2015
Although the latest polymeric drug-eluting stents (DES) have enhanced percutaneous coronary intervention (PCI) procedures, a substantial proportion of patients requiring percutaneous transluminal coronary angiography (PTCA) is elderly with numerous different comorbidities. This population requires use of effective DES that can minimise the risk of bleeding and/or thrombosis. Two symposia were held at EuroPCR, the official congress of the European Association of Percutaneous Cardiovascular Interventions, in Paris on 19–22 May 2015, with the objectives of sharing clinical experiences in the use of absorbable polymer stents and to understand why an absorbable polymer DES may be specifically indicated in PCI subsets such as chronic total occlusions (CTOs) or tortuous coronary anatomies. To meet these clinical challenges, a novel DES was discussed: Coracto™ (Alvimedica) is a DES with a unique design that elutes sirolimus from an absorbable poly(lactic-co-glycolic acid) (PLGA) polymer.
How to Ensure Procedural Safety and Good Long-term Results in Complex Coronary CTO Procedures
Professor Ahmed Khashaba of Cairo, Egypt presented the factors that should be considered before performing a CTO procedure. First, it is essential to select the right patient, keeping in mind that the expected benefit of a CTO procedure must exceed the negative consequences. It is also important to take the age of the patient into account, as well to assess the level of anti-ischaemic medical therapy received, the symptom status and the ischaemic burden. According to current guidelines, percutaneous recanalization of CTOs should be considered in patients with expected ischaemia reduction in a corresponding myocardial territory and/or angina relief.1 In addition, retrograde recanalisation of CTOs may be considered after a failed antegrade approach or as the primary approach in selected patients. In a meta-analysis comparing successful and failed PCI for CTO, successful PCI recanalisation of a CTO was associated with improved long-term clinical outcomes.2 In another meta-analysis, successful recanalisation was associated with a significant reduction in the rate of residual/recurrent angina.3
Good preparation is essential for performing CTO procedures. Preprocedural imaging should include myocardial perfusion imaging to assess ischaemia and myocardial viability, and multiple detector computed tomography to determine the 3D vessel course in the occluded segment, the length and composition of the CTO, and the distal vessel size and remodelling. Pre-procedural medications should comprise standard dual antiplatelet (DAPT) and anti-ischaemic therapy. Strategies to prevent contrast-induced nephropathy should also be considered; these include discontinuing any nephrotoxic drugs, intravascular volume expansion and administering a predefined maximum radiographic contrast dose (4 ml x body weight [kg]/serum creatinine [mg/dl]).
Radiation dose management is essential as radiation injury can lead to severe consequences for the patient, ranging from erythema that resolves in hours to ulceration that can take >6 weeks to heal; therefore, the patient should not undergo a repeat procedure prematurely.
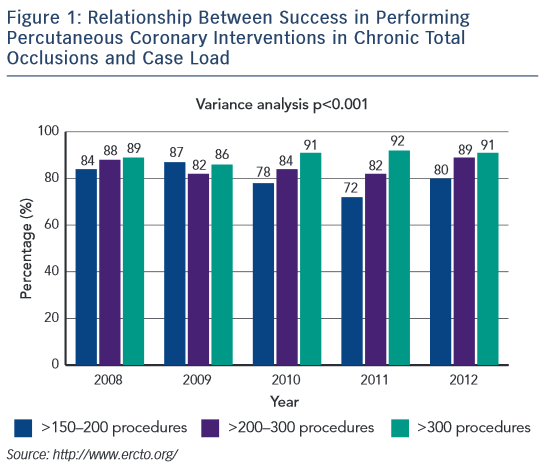
It is also important to tailor the case selection to the level of experience of the operator. A Level C operator (i.e. having undertaken <500 PCIs) should only perform PCI of simple lesions and simple bifurcations. A Level B operator (500–1000 PCIs) may perform more complex procedures including PCI of complex bifurcations, moderate calcified lesions and some cases of CTO. Only a Level A operator (>1000 PCIs, including ≥300 CTOs) should be permitted to perform PCI of difficult cases such as long and highly calcified lesions and complex CTOs, including retrograde approaches. If a Level C operator attempts a Level A task, he/she is less likely to be successful and may cause harm to the patient.4 Data from the European CTO registry shows the correlation between success rate and case load in performing PCI for CTOs (see Figure 1; http://www.ercto.org/).
Another essential factor in assuring success with CTO procedures is the use of the appropriate approach. A bilateral femoral approach gives a larger lumen for more equipment and better support, but has a higher rate of vascular complications. A bilateral radial approach results in a smaller lumen, less support, higher radiation exposure, but has a lower rate of vascular complications and better patient comfort. A combined femoral and radial procedure is the optimal approach, using a larger sheath/guide than when using an antegrade approach.
It is essential to exert minimal disruption during the PCI procedure. A study assessing the incidence of reocclusion and identification of predictors of angiographic failure after successful CTO, found that a successful subintimal tracking and re-entry technique was associated with a 57 % reocclusion rate.5 However, the use of everolimus-eluting stents was associated with a significantly lower reocclusion rate.
The immediate outcome should be optimised – a final thrombolysis in myocardial infarction flow < grade 3 (TIMI <III) is associated with lower major adverse cardiac event-free survival rate.6 A recent study found that the use of intravascular ultrasound (IVUS)-guided intervention leads to increased post-dilation, balloon pressures and post-procedural minimum lumen diameter, and improved clinical outcomes compared with conventional angiography-guided approaches.7
Finally, stent choice for CTO interventions is crucial; second-generation DES are associated with lower rates of restenosis and re-occlusion compared with first-generation DES.5,8–10 An ideal stent for a complex CTO intervention would be a biodegradable polymer or polymer-free DES with thin struts and vessel conformability, thus resulting in good vessel coverage, low or no longitudinal stent deformation and low restenosis rates.
In conclusion, appropriate pre-procedural planning is key to ensuring high success rates and avoiding unnecessary risk. Optimising the immediate outcome is essential to maintaining long-term patency. This may be facilitated by minimal vessel disruption, and the use of IVUS and second-generation DES. Currently available DES with absorbable polymer may further improve device safety and efficacy.
Live Case Demonstration
In order to illustrate the points discussed, a live case was presented from the Institut Cardiovasculaire Paris Sud, Massy, France. The patient was a 56-year-old man with hypertension and hyperlipidemia, and he was an ex-smoker, but had an active lifestyle. The patient had a history of obstructive sleep apnoea and ischaemic heart disease with inferior ST elevation in 2007, when he underwent implantation of a bare-metal stent (BMS) into the left circumflex artery (LCX). In 2012 he had a negative MRI stress test. He presented with 3 months of dyspnoea and a positive MRI stress test in April 2015. At this time his renal function was normal. An ECG showed evidence of the previous infarct. An echocardiogram showed focal hyperkinesis with normal pulmonary pressures and there was a positive MRI for ischemia in the atrial septal regions; the injection fraction was normal in the two-chamber view; and focal anteroseptal and apical ischaemia were detected in 4 of 17 segments. A delayed perfusion scan showed evidence of the previous infarct. The cranial view on angiogram showed proximal left anterior-descending artery (LAD) occlusion with a tapered proximal cap. The right coronary artery (RCA) also showed proximal stenosis.
A biradial antegrade approach was used from the left radial artery to the RCA, with the aim of minimising the risk of bleeding complications. The occlusion was a CTO of approximately 10 mm with a J-CTO score of 0 or 1. An antegrade microcatheter approach was taken to penetrate the proximal cap using soft wire, thus minimising the use of a contrast agent. A double injection was used. Little ischaemia was evident but a proximal LAD occlusion was seen. The Gaia guidewire was rotated rather than pushed into the cap. The proximal section was relatively easy to cross but the distal section was more difficult. The wire was withdrawn and re-entry attempted but it was not possible to cross the lesion with a microcatheter. To stabilise the catheter, trapping with a balloon was considered the safest approach. At the second attempt, the wire still did not move freely but managed to cross the occlusion. However, difficulty was encountered in crossing the occlusion with a balloon. An anchoring technique was then used to support the guide. The guidewire was changed and a subsequent predilation with a 2.0 balloon proved easier. However, the lesion was so calcified that the predilation was not fully successful, therefore a 2.5 balloon was used, up to 20 atmospheres. A single Coracto stent was implanted and IVUS confirmed that the outflow was good. DAPT was planned for a maximum 6 months. If the patient tolerates DAPT and is doing well, there is no need to stop early.
PCI in a Patient with a Complex Coronary CTO: Procedure and Clinical Outcome
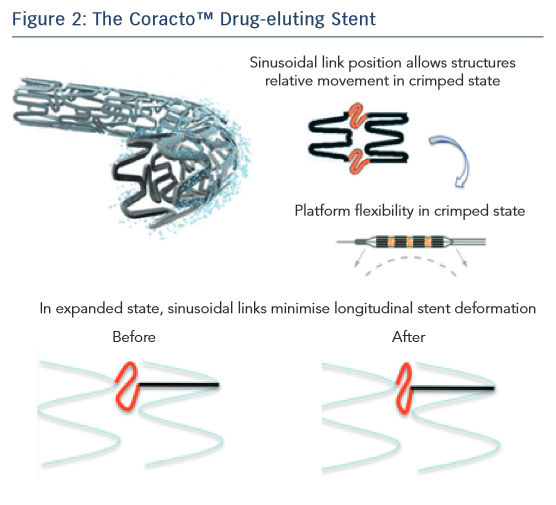
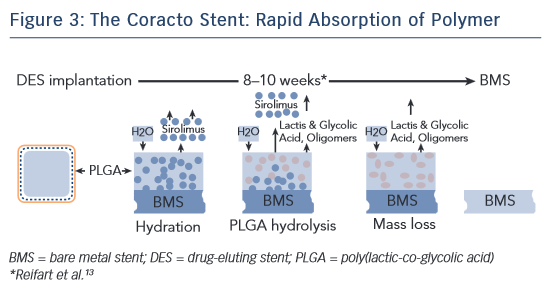
Dr Roberto Garbo of Turin, Italy began his presentation by stating that the availability of DES has greatly improved outcomes in CTO, as the use of BMS has been associated with revascularisation and restenosis. However, a DES has specific requirements when treating CTO; these include deliverability, stent matching to the vessel and good clinical results at follow-up. In terms of delivery, the Coracto DES features optimised geometry in the ‘crimped’ state owing to its sinusoidal link position that allows flexibility (see Figure 2), thin stent struts (a total strut thickness of 88 μm, lower than other currently available DES) and an optimised delivery system. Next, Dr Garbo considered stent matching to the vessel. The Coracto DES also features optimised geometry in its expanded state, a result of its sinusoidal link shape. Another important consideration is elastic recoil, i.e. the natural reduction in diameter of the stent after deflation of the balloon due to the elasticity of the stent material. Most DES are formed of cobalt-chromium, which has an average recoil of 5–6 %. The Coracto DES is made of stainless steel, which has an average recoil of only 2–3 %.11 Stent recoil has been identified as a significant predictor of late lumen loss (LLL).12 Longitudinal stent deformation is also a crucial factor in matching a stent to a vessel. The sinusoidal shape of the links in the Coracto stent minimises longitudinal deformation. The stent has a maximum expanded cell diameter of 4.0 mm, making it ideal for side-branch crossing.11 Finally, the Coracto DES is designed to optimise clinical outcomes. Preclinical studies indicated that the polymer of the Coracto DES provides controlled release of rapamycin (sirolimus), and degradation of the polymer is completed within 8–10 weeks, leaving a BMS (see Figure 3).13
Dr Garbo presented a case of a 75-year-old man with effort angina and moderate antero-lateral ischaemia identified by single-photon emission computerised tomography. A basal angiogram showed LAD ostial occlusion with some collateral flow from the right. The blunt CTO segment and occlusion length of >20 mm resulted in a J-CTO score of 2, which indicates a difficult procedure with reduced success rate (<90 %).14 Treatment of the CTO was by PCI of the ostial LAD with a bilateral femoral approach using a Fielder XT-A guidewire and a Corsair 135 catheter. A contralateral injection was performed to confirm entry into the true lumen, followed by predilation with the microcatheter. IVUS was also used to evaluate the left main (LM) artery. Two stents were implanted: a Coracto 3.0 × 24 mm and a 3.5 × 17 mm on the LM artery. Proximal optimisation technique was performed in the LM artery with an NC 4.0 balloon and a triple kissing balloon 3.5–2.5–2.5 was also needed. Final IVUS confirmed the success of the procedure. At 9 months’ follow-up, angiography and optical coherence tomography (OCT) were performed. Good endothelialisation of all stents was seen with mild in-stent restenosis on the worst area of occlusion (LLL: 0.39 mm).
In conclusion, complex CTO recanalisation is easier to achieve when using the most appropriate method (e.g. controlateral injection for the visualisation of distal vessels) and adequate materials (microcatheters and dedicated wires). The Coracto DES has unique properties that make it a useful option in treating such challenging lesions, including rapid reabsorption of polymer. It has demonstrated a good safety profile, showing complete endothelialisation of all struts at follow-up OCT evaluation.
PCI in a Patient with a Complex Coronary Anatomy: Procedure and Clinical Outcome
Dr Kursat Tigen, of Istanbul, Turkey discussed the challenges of PCI in complex coronary anatomy, which includes unprotected LM stenosis, bifurcation lesions, CTOs, long lesions, diffuse lesions, severe calcification and tortuosity, and thrombotic and undilatable lesions. Atraumatic delivery and precise positioning of a stent across the target lesion are the most basic requirements of a successful intervention. This requires careful preparation, including selection of the access site, guiding catheter (type, size and curve), guidewire and dedicated devices for lesion crossing, as well as a planned procedure, including the decision whether to perform predilation, direct stenting and single- or double-stent strategy. The need for surgical back-up and pharmacotherapy to reduce the risk of thrombotic complications should also be considered.
Stent selection is an important part of planning an intervention, with the aim of avoiding procedural failure. Unfavourable mechanical properties of stent delivery systems such as rigidity, poor deliverability and crossability can reduce the success rates in complex coronary PCI procedures. Resistance to longitudinal deformations is also important and is influenced by strut thickness, connector number and design. The open-cell design is preferred to increase the flexibility of the stent at the expense of reduced radial force. The mechanical response of coronary stent systems has been described using terms such as pushability, trackability, crossability, flexibility and conformability. Each of the three delivery parameters (pushability, trackability and crossability) is based on the resisting forces that can be quantified along the delivery path.
Pushability represents the transmission of the applied force to the catheter tip, and hence ‘feel’ of the operator. The bending stiffness of the stent system also contributes to the pushability. Bending stiffness is a measure of the structure’s resistance to bending deformation and is the reciprocal of flexibility. Trackability is the ability of stent delivery system (SDS) to track or move easily through the curved vascular pathway. The ability of the SDS to bend and twist will most likely depend on the geometry of the connections and raw material. Low tracking forces are necessary to prevent stent dislodgement or mechanical vascular injury. Crossability is the ability of SDS to pass through the target lesion. Crossability depends mainly on the profile of the crimped stent. Low-profile SDS devices appear to be essential in cases with extremely tight and complex target lesions. Flexibility is critical in preservation of the function and the integrity of the stent in complex coronary interventions. Flexible stents are easily inflated and show great adaptability to vessel shape compared with a rigid stent. The ability of a stent system to conform to the geometrical shape of the vessel after stent implantation is defined as conformability. Stent conformability is associated with efficient and homogeneous diffusion of the anti-proliferative drugs in the coronary vessels. Stents with biodegradable polymer technology are also desired devices for complex lesions as they have been associated with lower rates of late stent thrombosis.
To illustrate these factors, Dr Tigen presented the case of a 50-year-old man who had exercise angina (Canadian Cardiovascular Society Grade III) and dyspnoea. He had arterial hypertension, diabetes and a family history of coronary artery disease, and had been a smoker for 40 years. Echocardiography showed inferior hypokinesia with preserved ejection fraction, as well as mild mitral regurgitation. The angiogram showed mild proximal LAD disease but severe stenosis in the body and the side branch of the LCX artery. The RCA also had sub-total occlusion from the proximal to the distal end of the vessel; this was a long lesion. Fractional flow reserve measurement of the proximal LAD disease revealed a haemodynamically non-significant lesion (basal: 0.89; maximum hyperaemia: 0.81). The procedure was carried out with PCI to the complex RCA lesion. Peri-procedural management included a loading dose of 300 mg clopidogrel and 100 mg aspirin, and 8000 IU heparin for anti-coagulation. A right femoral approach was selected with a 7F sheath, a JR4 AlviguideBlue+ guiding catheter used for coronary engagement and a BMW Universal 0.014 inch guidewire was used for lesion crossing. This passed the lesions easily despite marked complexity. Predilation was performed using a 1.25 x 15 mm balloon, then a 2.0 x 20 mm balloon. Stenting was performed using a full-metal jacket procedure from the proximal segment of the postero-lateral branch to the osteal RCA. A 2.5 x 28 mm Coracto DES was followed by 2.75 x 28 mm, 3.0 x 32 mm and 3.0 x 21 mm Coracto DES, and the procedure was finalised with 3.0 x 15 mm non-compliant balloon postdilation up to 24 atmospheres. The final angiogram revealed good stent expansion and strut coverage with a TIMI-III flow. Despite severe tortuosity and calcification, the stent conformability was excellent. One year angiographic follow-up demonstrated an intact RCA with all stents open and no significant restenosis.
In addition to the favourable mechanical properties increasing the success rate, such as stent design, thin struts and low polymer thickness, resulting in a DES that is easy to manipulate, several factors influenced the choice of Coracto DES in this complex coronary procedure. Its 100 % absorbable (PLGA) coating is quickly absorbed, assuring no long-term inflammation with optimised endothelialisation and reduced rates of stent restenosis. Controlled elution of sirolimus is also associated with excellent efficacy in terms of anti-proliferative properties.
In challenging endovascular anatomy, usually more than one important mechanical property of SDS and the stent platform may come in to play. In practical terms, the design of the Coracto DES presents numerous advantages in complex coronary interventions. Greater pushability is useful for small vessels and diffuse atherosclerotic disease with narrow proximal access. Good trackability and flexibility are beneficial in diffuse or calcified lesions, highly tortuous proximal vessels and distal target lesions. Furthermore, a high demand on crossability is required in cases with tight and complex target lesions. Finally, stent conformability is essential in homogeneous diffusion of the anti-proliferative drugs in the coronary vessels.
In conclusion, the Coracto DES is a safe and effective option in PCI of complex coronary anatomy cases with high procedural success rates and long-term beneficial effects.
Summary and Concluding Remarks
These presentations have highlighted some important unmet needs in PCI interventions. In complex clinical cases such as CTO and full-metal jacket procedures, the Coracto stent’s unique structure and rapid polymer absorption offers excellent conformability, efficacy and safety.